About Our Clinic
The California Cranial Institute exists to heal the planet,
one body, one mind, and one spirit at a time
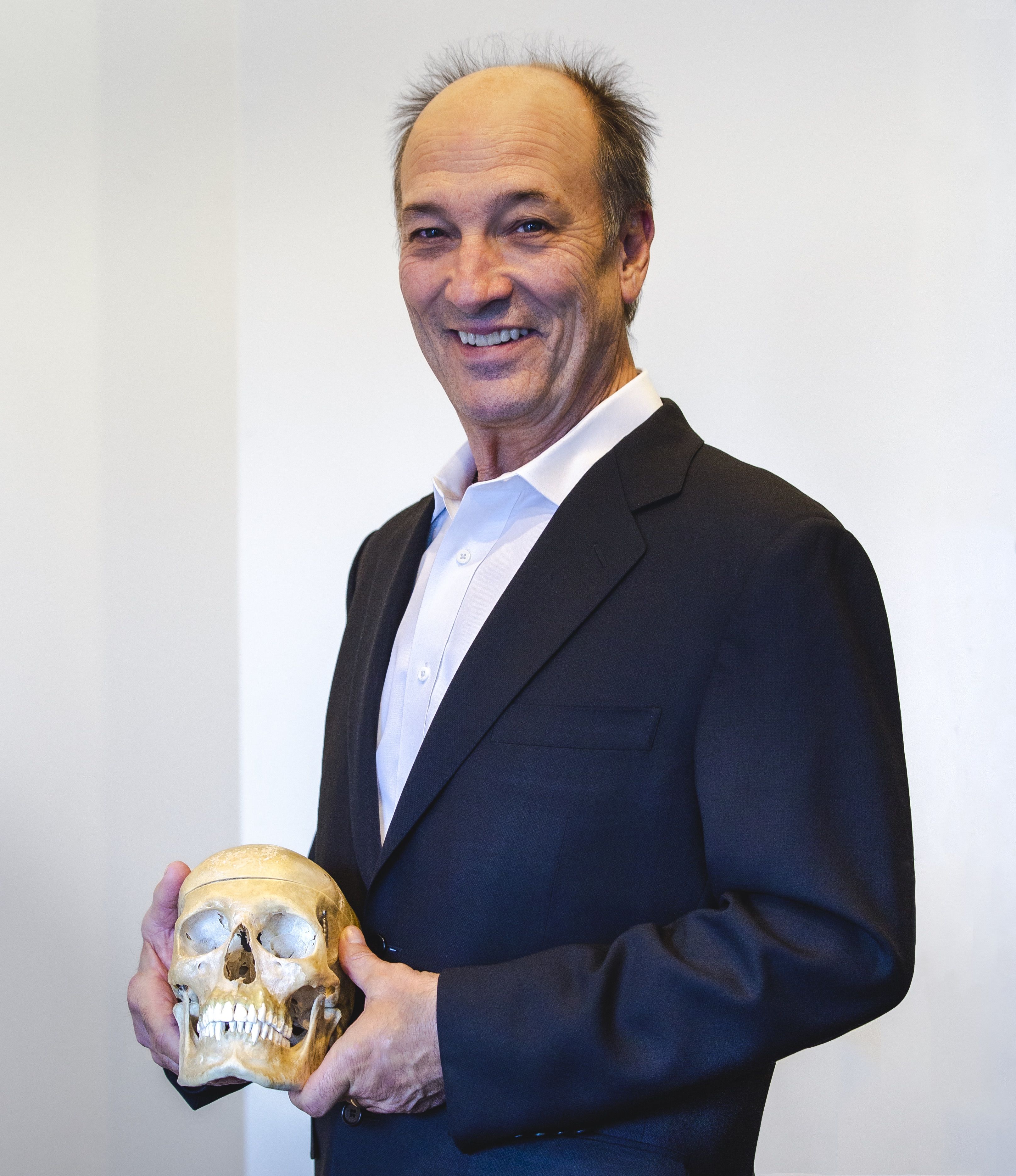
Dr. Bloink is a board-certified Craniopath, a specialist in Cranial Dental integration, and a certified Neuro Emotional Technique practitioner. Because of his skills and techniques used to improve ones’ quality of life, teaching experience, conference presentations, and eminent research, he is frequently asked to give lectures to doctors across the country and around the world.
Learn More
An Integrative Multidisciplinary Approach to Healing
Conditions We Treat
No matter where you are coming from we will do our best to make you comfortable and cared for. At the California Cranial Institute we treat a variety of conditions:











